(NB: The 3 parts will make more sense if they are read in order …)
In Part 1, we considered the increased risk of cesarean delivery with the universal practice of 39 weeks induction. In Part 2, we tried to determine whether that strategy would result in fewer fetal losses and how many. Overall, it seems clear that many fetal losses could be saved but that this would come at the expense of increased maternal death and other unintended consequences from increased numbers of cesarean deliveries.
Yet cold hard numbers usually don’t tell the whole story about why humans make certain choices. Values do. People have different values, and every day folks choose to do things that might seem “unsafe” to others because it makes them happy. How do we quantify or weigh these considerations, that is, our patients’ values? The debaters do not account for the potential value to the patient of going into spontaneous labor and/or having her baby in a natural way. How can we measure this seemingly intangible value? Or is that even our job? Perhaps our job is to inform patients of the risks and benefits of a particular strategy and let her filter that in view of her values.
Consider this: there is no value or benefit derived from eating hot dogs and there’s some evidence that eating hot dogs may increase your risk of colon cancer, pancreatic cancer, and even prostate cancer. Of course, the absolute increased risk is infinitesimally small (even if these risks are real). But if we assume that even one person per some large number of people develops cancer from hot dogs, while, on the other hand, there’s absolutely no value in eating hot dogs, then, using our debaters’ logic, we should conclude that hot dogs should be made illegal in the United States. In fact, there is a group of about 12,000 doctors who have made this argument. So why would anyone ever eat a hot dog? The intangible value in eating hot dogs is that they taste really good and some of us are willing to take some risks to eat something tasty.
But here is a better example: What about breasts? We have an epidemic of breast cancer today in the United States. American women have a 12.4% risk of developing breast cancer at some point in their lives. Around 246,000 women each year are diagnosed with breast cancer and over 40,000 women die every year from it. Hundreds of thousands of women undergo invasive surgeries, chemotherapy, and other treatments. The sad part is that nearly all of this is preventable. If every woman, as soon as she is done with her childbearing and breastfeeding days, at an average age of about 30, were to have simple, prophylactic mastectomies, we could potentially save the lives of over 40,000 women a year, and prevent many more women from undergoing radical and expensive treatments for breast cancer. How many millions of women would rest easier each night not having to worry about breast cancer?
The prophylactic mastectomy itself, performed on a young healthy woman, is a very safe procedure. It’s much better to do a mastectomy on a healthy 30-ish year old woman than it is on a less healthy, cancer-stricken woman in her 60s or 70s. The surgeries would go off without a hitch with very few complications, and the more we did in the US then the better we would get at doing them. It would quickly become an inexpensive and very low risk procedure, much like circumcision. Overall, our healthcare system would save money, eliminating huge numbers of interventions and screenings, reducing lost time at work, prolonging productive life years, etc.
And why not do it?! Once a woman has concluded her breastfeeding years, what purpose do breasts serve? They are of no value to anyone. They are just ticking time bombs, killing over 40,000 women a year in the prime of life. Breasts kill thousands more people each year in the US than do guns.
This is the same argument our debaters make when they claim that spontaneous labor is of no value to any woman and that cesareans aren’t really that risky, etc. In fact, we could make a better and more rational argument that all women should undergo prophylactic mastectomy at age 30 than we can that all pregnancies should be ended at 39 weeks. Though my tongue is firmly in my cheek right now, I am not exaggerating the comparison. The number of lives saved through routine mastectomy is many orders of magnitude greater and the financial impact on the healthcare system overall is much more favorable.
So why not? Hopefully you feel uncomfortable even contemplating the idea that we might actually encourage this practice, and much of that discomfort likely comes from one statement: Breasts have no value to the woman or to our society. Unfortunately, our debaters believe that spontaneous labor has no value to women at a time when women are increasingly seeking alternative birthing options. Women are frustrated with a system of obstetrics that discounts their wants and values and seems to rob them of control over the process of birth. This attitude among obstetricians, which takes control away from the woman during her birth process, will increase the number of women who choose not to seek prenatal care at all; in turn this will increase the number of women who give birth at home, often with untrained birth attendants. This happens today when women attempt a trial of labor after cesarean (TOLAC) at home because they have encountered ignorant and dangerous attitudes at the obstetrician’s office, like, “Once a cesarean, always a cesarean.” The obstetrician who holds such attitudes sees no value in vaginal birth and, worse, doesn’t understand the scientific evidence about the risk/benefit ratio of repeat cesarean versus a TOLAC. Women and babies are being harmed as a result. These attitudes have to change. The rhetorical harm is even greater when women are told that they should cede all control of their birth process by two men having a “debate.” The inappropriate and perverse misuse of statistics to conclude the inconclusive is simply dangerous.
Of course, the values that women hold should be informed by facts. All of us are biased by our preconceptions, experiences, and values. The debaters too were influenced by their biases, viewing the same numbers from a different perspective than the next person might have. During this “debate,” Dr. Norwitz made the bold proposition, “Nature is a lousy obstetrician.” He was lamenting how horribly inefficient nature is at reproduction, with so much fetal wastage, mostly in the form of early miscarriages. He made it clear that he believes we can do better than nature.
But can we do “better” than nature? This is a philosophical point of difference that the debaters hold compared to many, including myself. It’s not really a question of doing better than nature when we seek to reduce perinatal death or maternal mortality, it’s more of a question of correcting abnormalities that sometimes come up in the course of an otherwise natural event. Is birth natural and wondrously efficient when it works as intended? Or should we seek to “improve” the natural state of our biology?
From a philosophical perspective, I would argue that we cannot do better than nature. To think that we can is an arrogant position, full of brash statements and overconfidence. We don’t even understand the pathways that lead to human parturition, and for that matter, we don’t really understand 99% of the disease processes we treat in medicine. We merely throw band-aids on things as they come up. We have had a significant impact in obstetrics over the last two centuries in reducing perinatal mortality, but we haven’t even scratched the surface in our understanding of human biology.
The philosophical question remains, Can we do better at making a baby than a woman who is otherwise in good health and has no environmental or genetic encumbrances? To think that we can is absurd. It’s one thing to recognize that sometimes infections or other abnormal processes may lead to preterm labor, and that we might be able to intervene and prevent preterm labor (though we haven’t really been able to do so far), but it’s another thing to think that we can improve on the natural process of human reproduction when it works correctly. Healthy pregnancies do not usually end at 39 weeks without intervention. At what point does a normal process become abnormal? If we assume that nature is likely to get it right, then we are left with a lot of unanswered questions when confronted with the prospect of delivering all women two weeks earlier. In what ways might we harm normal pregnancies by ending them almost two weeks earlier than nature intended? What might we learn 50 years from now about the value of later gestations? What epigenetic or hormonal triggers might we be altering? I don’t know and I certainly don’t want to overstate the potential harms, but my point is only that I don’t assume to be smarter than nature.
There is an irreducible amount of wastage in human reproduction which Dr. Norwitz decries as an imperfect nature that we must correct. This argument is full of idealism and optimism. Yet, the bulk of human wastage is related to genetic and chromosomal abnormalities, for which we do not now have and likely will never have either the treatments or the will to use such treatments to prevent those type of first trimester miscarriages. Let’s not give false hope to the women who suffer first trimester miscarriages due to chromosomal or genetic problems because we think that we are somehow smarter than nature and can prevent them.
This is the type of thinking that has led to useless interventions like progesterone supplementation, or worse, DES. DES was a miracle drug devised to combat fetal wastage by a generation of scientists who thought that they too had out-smarted nature. Physicians embraced DES because they really didn’t understand the scientific evidence of its efficacy but the bias that we can outdo and overcome nature drove this unwarranted adoption and skewed how physicians interpreted the available evidence. When DES was adopted, we didn’t know the cause of these first trimester losses. Decades later, the idea seems silly to us, though physicians still use progesterone supplementation with no evidence of benefit. How silly will we look 50 years from now when future generations wonder with skepticism why we thought the answer to preventing fetal losses was earlier delivery at the expense of an increased cesarean delivery rate? Ultimately, we are sliding off a slippery slope (an example of therapeutic drift), and universal delivery at 38 or even 37 weeks will be the next suggestion for prevention of IUFDs.
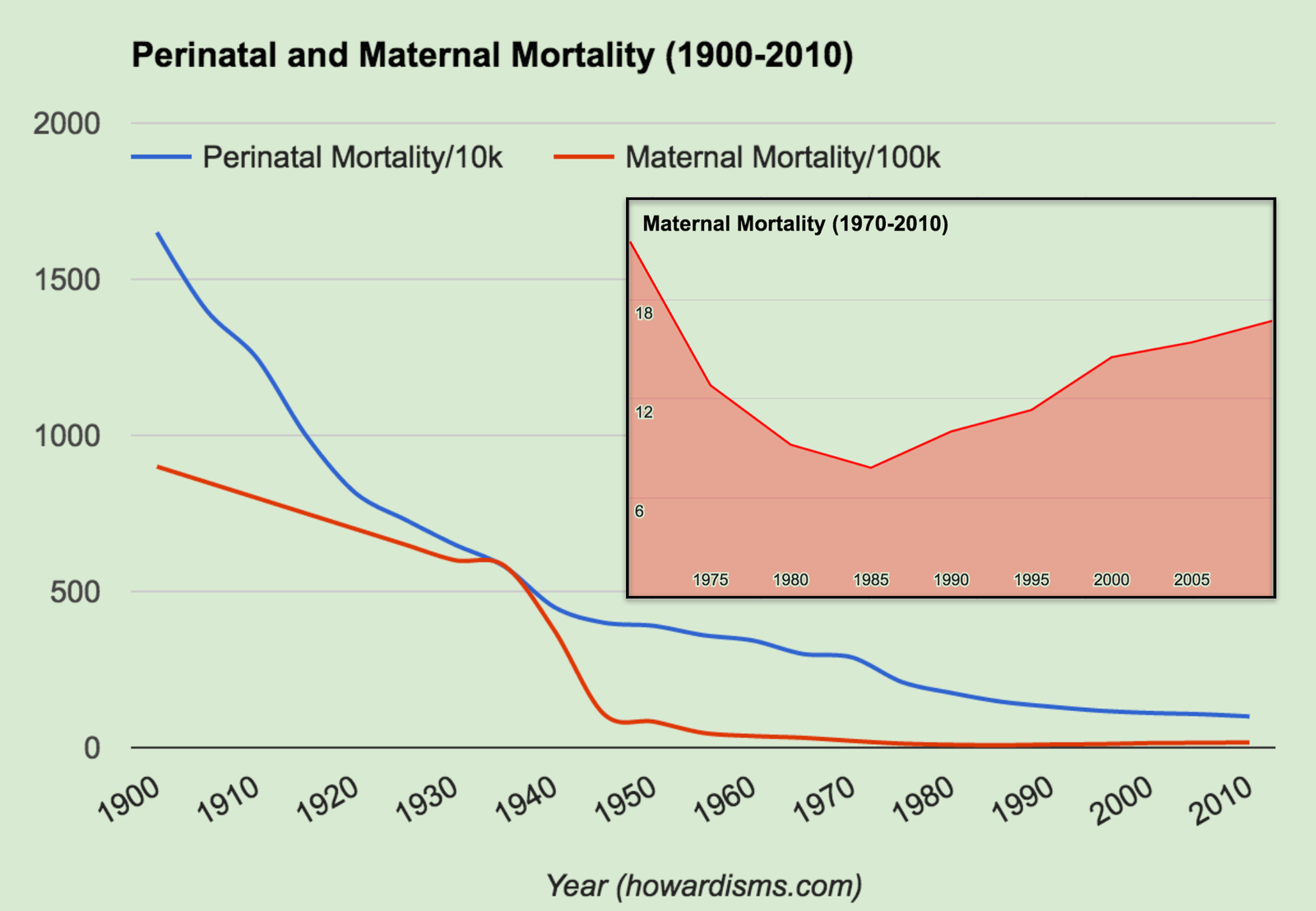
One hundred years ago, physicians felt that they had conquered nature and surpassed it. As the 20th century rolled on, with the emergence of antibiotics and the other miracle drugs and technologies, this egotistical view of what we do was further solidified. Nevertheless, we continue to make mistakes due to this arrogance, and not just of the DES-type. DES didn’t work and harmed women (transgenerationally as it turns out). But antibiotics work. Antibiotics were a wondrous and life-saving breakthrough, but their over-utilization might have disastrous implications for our future health. Safe cesarean delivery is perhaps the most important breakthrough in obstetric history, yet its over-utilization is now leading to unacceptable increase in maternal mortality, which rose almost 80% between 1987 and 2010 (see the graph above). We reached the lowest point of maternal mortality in 1987, over 99% lower than 100 years before, but have been trending upwards ever since. As a side note, in 1991, the Health People 2010 report called for a goal of a maternal mortality rate of 3.3/100,000. Instead, it was 16.7/100,000.
We don’t think of debates about numbers as being influenced by philosophy or bias, but unfortunately this is almost universal. Issues like these should be analyzed with Bayesian probabilistic reasoning or inference. Questions this complex are not answerable with Frequentist methods, which are all too easy to pervert. “Lies, damned lies, and statistics,” is very much a reflection of the misuse of Frequentist methods. R.A. Fisher, the father of Frequentist statistics, famously used his statistical tools to show that the conclusion that cigarette smoking causes lung cancer was wrong. He argued that when a person has lung cancer, it drives them to smoke (due to irritation). How could he be so wrong? He misused statistics due to his own biases: he was a smoker himself, and he loathed the fact that Bayesian inference had been used to prove the link between smoking and cancer. This interesting footnote of history should serve as a warning to those who continue to use his methods to make similar mistakes.
Philosophy not only biases our interpretation of data, but it influences how we present that data to patients. Obstetrics has moved away from valuing the life of the mother as more important than the life of the fetus. We generally present information to a mother in a way that forces her to say that she would rather risk her own life to save the baby’s life. What mother wouldn’t? But these are not usually 1:1 exchanges. Would a mother increase her risk of death by 1% to decrease the risk of death for the fetus by 0.001%? It depends on how the data is presented to her. Perinatology often forgets about the mother – focusing instead on the fetus – even though perinatal interventions, like ultrasound, are of little to no value overall.
Obstetricians today are spoiled by not having to deal with maternal death on a more frequent basis; yet, they do encounter fetal wastage (mostly through miscarriages) almost daily. This has forced a change in emphasis. In 1850, women had about a 1 in 8 chance of dying in their lifetimes due to childbirth, and obstetricians often employed fetal destruction in order to save the life of a woman. Today, we have the luxury of relegating those practices to the past, largely due to cesarean delivery. Many obstetricians have never taken care of a woman who died in childbirth. Influenced by medicolegal concerns and a false sense of safety, obstetricians perform cesareans nonchalantly for almost any reason at all. I view this as hypocrisy, to care so little about the harms we do to women through our interventions, couched in the claim that we are benefiting the fetus. Many obsetricians believe that we have invented a better way to give birth, through cesarean delivery. But like any intervention, too much of a good thing is bad thing. Cesarean deliveries are like a defibrillator: they are great when you need them and potentially deadly when you don’t. We do not need to fundamentally change human birth.
There is a subtle difference between improving upon nature and intervening when things go wrong. Let’s not lose sight of our real job.